Vous êtes ici : UFR Simone Veil - santéFRFormation continueUltrasound examination of the venae cavae01. Superior vena cava
- Publié le 9 février 2023
- Version PDF
01. Superior vena cava
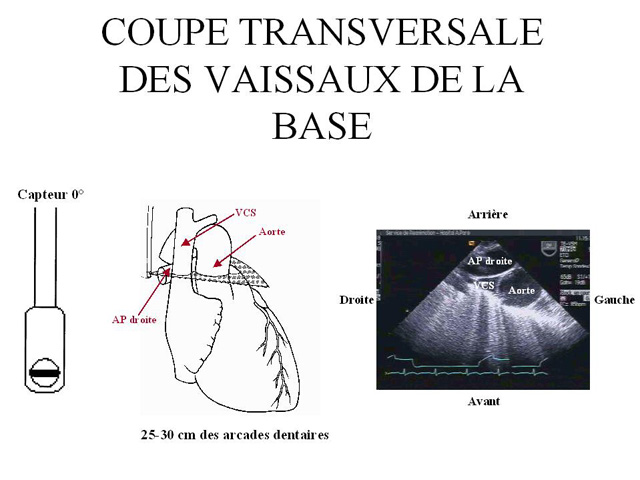
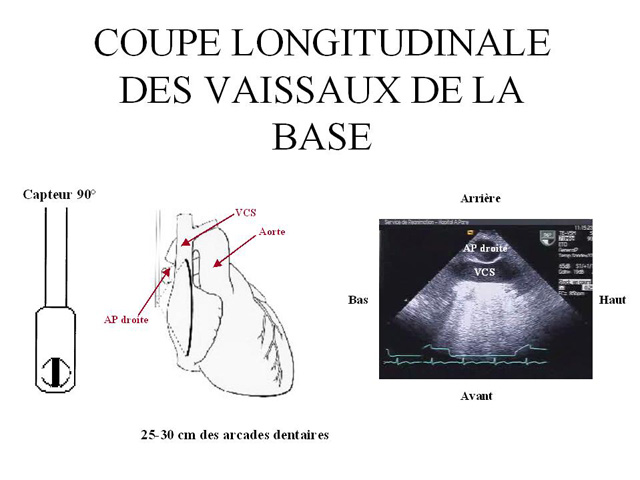
Echocardiography of the SVC can be done by a transesophageal approach (3).
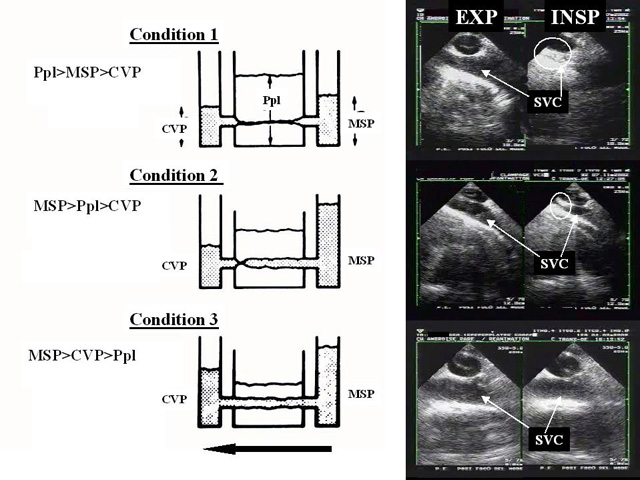
To remain open, this collapsible vessel must be subject to a distension pressure higher than the critical closing pressure. In a mechanically ventilated patient, the inspiratory phase raises the right atrial pressure less than the pleural pressure.
As a result, the difference between these two pressures, the SVC distension pressure, decreases in the inspiratory phase of assisted respiration and may become insufficient to keep the SVC open in a hypovolemic patient.
Because of an increase in pleural pressure, the SVC behaves like a Starling resistor, and the influence of the external pressure on its diameter is determined by the zone conditions.
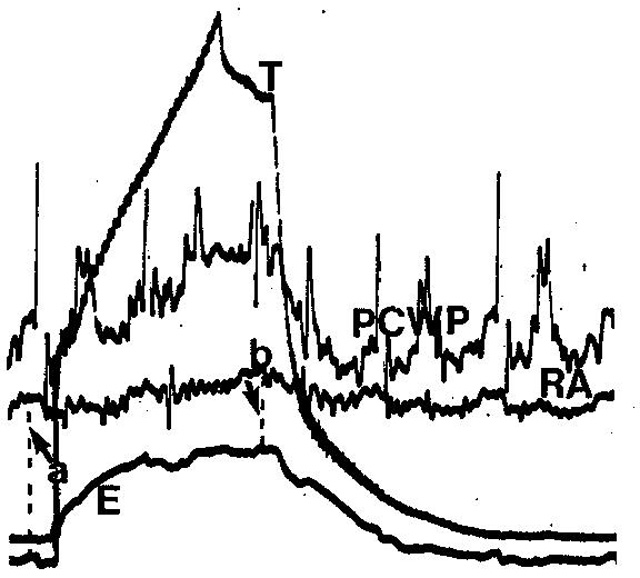
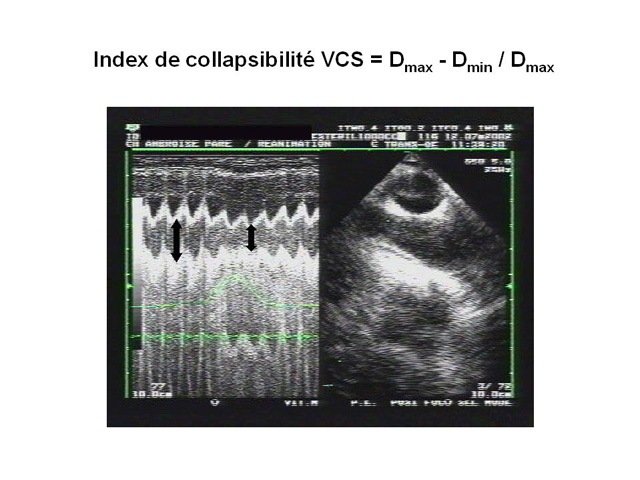
We have proposed the use of an SVC collapsibility index calculated as the difference between the maximum expiratory diameter and the minimum inspiratory diameter, divided by the maximum expiratory diameter.
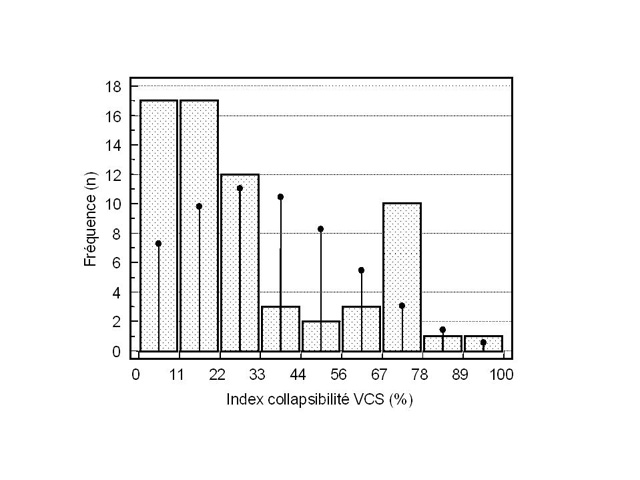
This index can be used to predict the response to fluid administration to a mechanically ventilated patient presenting with signs of circulatory insufficiency (4). This evaluation requires a long-axis view of the SVC (longitudinal view) using a multiplane transesophageal probe (figure 2), operating in two-dimensional M-mode. Our measurements in 66 septic shock patients showed that a collapsibility index above 36% predicted, with 90% sensitivity and 100% specificity, a positive response to volume expansion, marked by significant increase in cardiac flow (4).
In the same study, we observed a bimodal distribution of collapsibility indices, most patients experiencing complete, or almost complete, inspiratory collapse, or, conversely, presenting with insignificant inspiratory variations in SVC diameter .
We feel that this confirms the parallel drawn with a Starling resistor, which obeys the all-or-nothing rule.
Media
INSP: inspiration; EXP: expiration