Vous êtes ici : UFR Simone Veil - santéFRFormation continueUltrasound examination of the venae cavae02. Inferior vena cava
- Partager cette page :
- Version PDF
02. Inferior vena cava
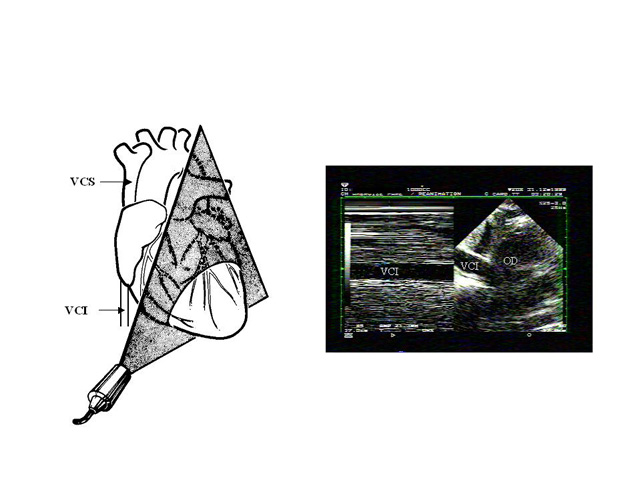
Echocardiography of the IVC can easily be done by a transthoracic, subcostal approach (5,6).
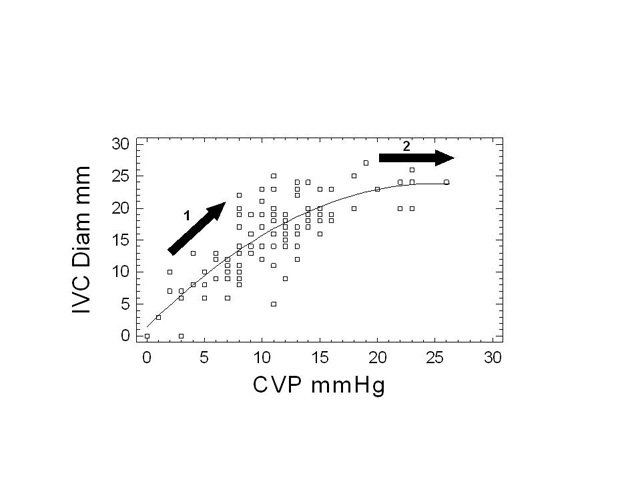
Measurement of IVC diameter in different positions differentiates normal subjects from patients with elevated right atrial pressure (7). In their famous study of venous return in the dog, Guyton and collaborators showed that venous return is improved by a moderately negative right atrial pressure, but is hindered by more negative right atrial pressures (8). Guyton explained this in terms of collapse of the IVC at its entry in the thorax, illustrating the inability of a collapsible vessel to transmit negative pressure (8). In work on severe asthma, we provided the first demonstration of the reality of this phenomenon in human subjects (9).
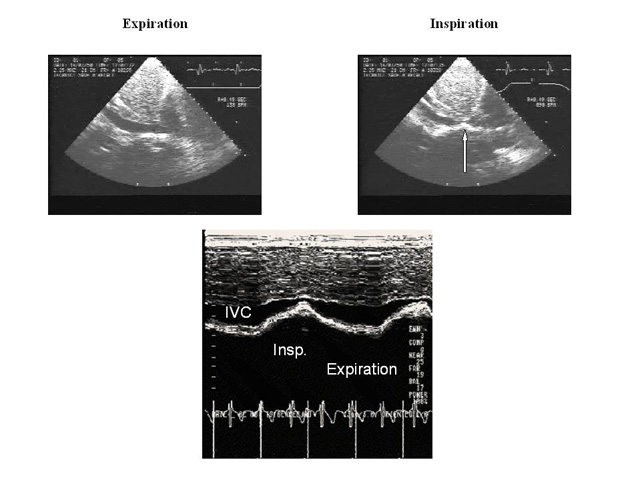
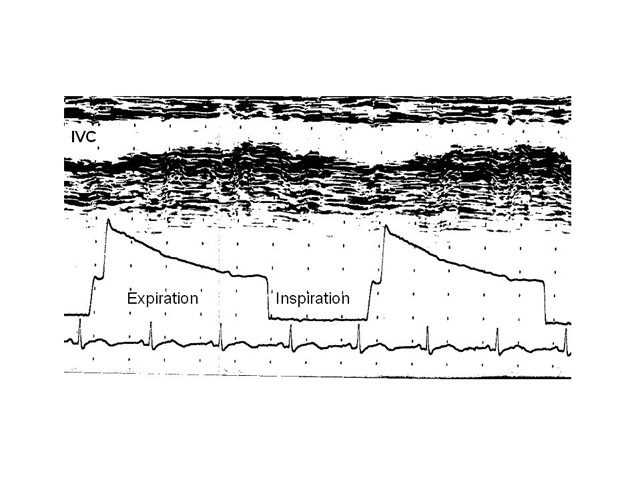
In a spontaneously breathing, healthy subject, cyclic variations in pleural pressure, which are transmitted to the right atrium, produce cyclic variations in venous return, which is increased by inspiration, leading to an inspiratory reduction of about 50% in IVC diameter (5).
When the IVC is dilated, the relation between the diameter and pressure is located on the horizontal part of the curve: respiratory variations in diameter, produced by a low inspiratory pressure, are therefore abolished.
This is what is seen in cardiac tamponade (10), and in severe right ventricular failure (6).
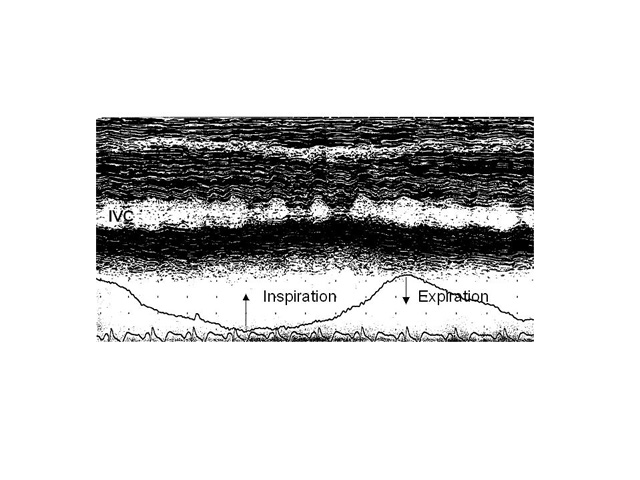
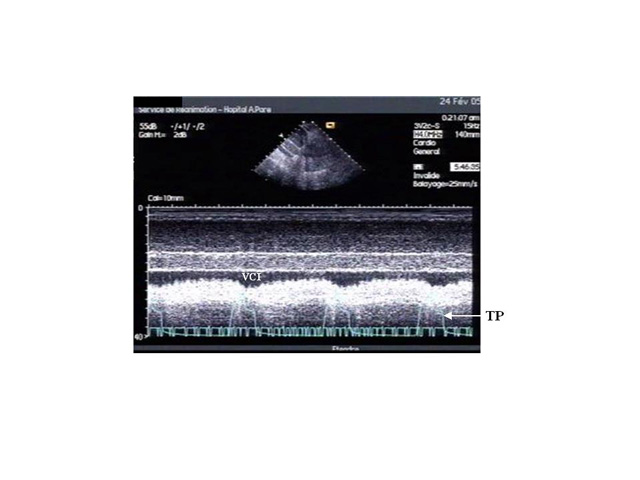
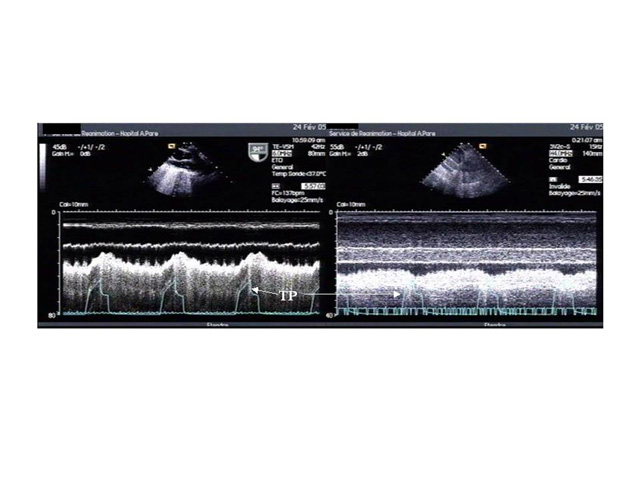
In a patient requiring ventilatory support, the inspiratory phase induces an increase in pleural pressure, which is transmitted to the right atrium, thus reducing venous return. The result is an inversion of the cyclic changes in IVC diameter, leading to increases in the inspiratory phase and decreases in the expiratory phase.
These variations are also abolished by dilatation of the vena cava, indicating high right atrial pressure for the same reason as before (figure 11). The respiratory variations in IVC diameter in a mechanically ventilated patient are therefore only observed when right atrial pressure is normal, that is low. In a patient presenting with signs of circulatory insufficiency, this finding may indicate hypovolemia. Measurement of IVC diameter in a patient receiving mechanical ventilation does not accurately predict right atrial pressure (11). Absence of respiratory variations in IVC diameter in a mechanically ventilated patient presenting with signs of circulatory insufficiency suggests that volume expansion will be ineffective in 90% of cases (12).
Feissel and collaborators were the first to propose using respiratory variations in IVC diameter to predict the response to filling in a mechanically ventilated patient (12). By expressing the respiratory variability in IVC diameter as the difference between the value of the maximum inspiratory diameter and the minimum expiratory diameter, divided by the mean of the two values, these authors showed that a 12% increase during the inspiratory phase differentiated patients likely to respond to vascular filling, in terms of increased cardiac flow, from those who would not respond, with a positive predictive value of 93% and a negative predictive value of 92% (12). The great merit of this work is that it proposes a dynamic, noninvasive parameter to evaluate the potential benefit of volume expansion. Moreover, the examination of the IVC is particularly easy and can be done by someone with limited experience in echocardiography. Feissel’s findings were simultaneously confirmed by our team (13).
One question remains though: is this index still valid when the patients have a high abdominal pressure which limits variations in IVC diameter?
Another phenomenon observed in the IVC of a mechanically ventilated patient is retrograde flow, which is unrelated to tricuspid regurgitation and is caused by the cyclic compression of the right atrial wall by the lung.
This compression forces the blood in the atrium backwards, especially when it occurs during cardiac systole, whereas the closed tricuspid valve prevents anterograde flow (14). This retrograde flow is a major source of inaccuracy when measuring cardiac flow by the thermodilution method in a mechanically ventilated patient (14).
In conclusion, ultrasound examination of the vena cavae provides new, precise and easily determined indices of the expected response to volume expansion in a mechanically ventilated patient with circulatory insufficiency.
Media
Figure 10 : Physiological respiratory variations in IVC diameter in a healthy volunteer breathing quietly. IVC diameter decreases on each inspiration.