Vous êtes ici : UFR Simone Veil - santéFRFormation continueCardiorespiratory interactions00. Cardiorespiratory interactions
- Partager cette page :
- Version PDF
00. Cardiorespiratory interactions
Cardiorespiratory interactions were long limited to research, which admittedly was fascinating but apparently had no major clinical applications. In recent years, and in the light of several publications, it appears that these interactions can in fact be used to develop tools for hemodynamic monitoring in ventilated patients, and even to adapt the ventilation parameters in certain ventilated patients, in ARDS for example. These interactions are the result of cardiopulmonary anatomy: the cardiac chambers are subject to intrathoracic pressure, the right ventricle branches upstream of the lung, the two ventricles have a common wall, the interventricular septum.
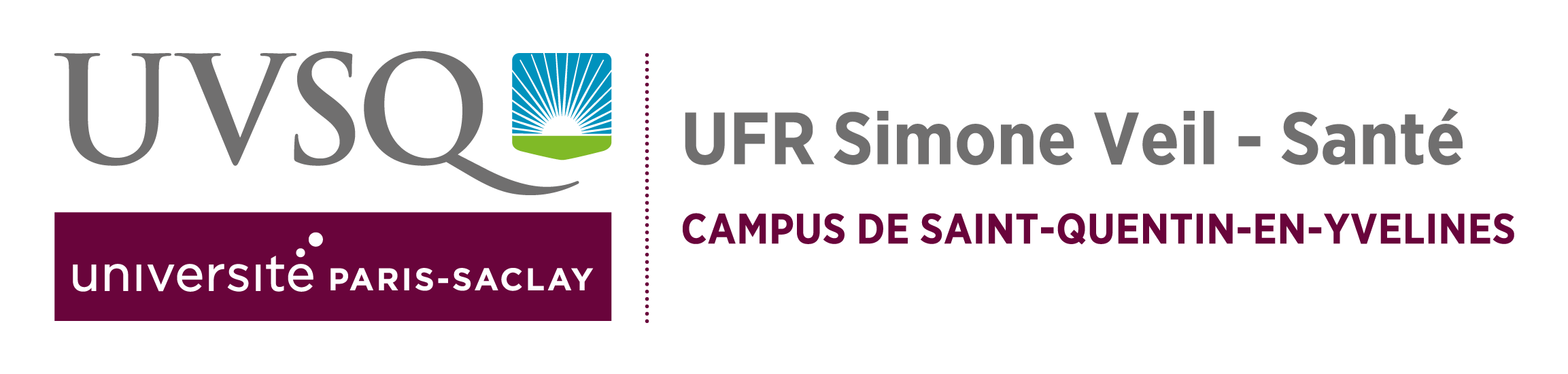
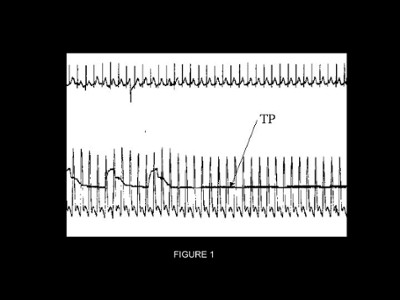
The cyclic variations of the pulse in mechanical ventilation were described in 1973 by Massumi et al. using the term reversed pulsus paradoxus. They comprise an inspiratory increase in systemic pulse. This increase may be absolute, and certain authors subsequently called it dUp (Figure 1). But it may simply be related to the drop in pulse described on expiration, and called dDown (Figure 2). It is only possible to make this distinction by disconnecting the patient from the respirator or by making a prolonged end-expiratory pause.
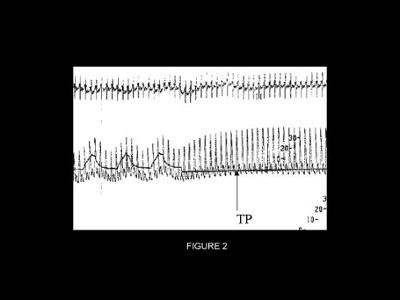
Doppler echocardiography is perfectly suited to the study of the mechanisms underlying these pulse variations. It can be used to investigate cardiac function parameters and to localize each heart beat in the respiratory cycle. For this, it is necessary to display the airway pressure signal on the screen of the echocardiograph. By convention, we have defined heart beat 1 as occurring at the end of expiration, heart beat 2 at the start of insufflation, heart beat 3 at the plateau, and heart beat 4 at the start of expiration.
Whereas at steady-state, and throughout the respiratory cycle, the stroke volume (SV) of the left ventricle is on average identical to that of the right ventricle, mechanical ventilation dissociates these two values: the SV of the right ventricle is decreased on insufflation whereas the SV of the left ventricle is increased at the same time.
The cyclic variations of the pulse in mechanical ventilation were described in 1973 by Massumi et al. using the term reversed pulsus paradoxus. They comprise an inspiratory increase in systemic pulse. This increase may be absolute, and certain authors subsequently called it dUp (Figure 1). But it may simply be related to the drop in pulse described on expiration, and called dDown (Figure 2). It is only possible to make this distinction by disconnecting the patient from the respirator or by making a prolonged end-expiratory pause.
Doppler echocardiography is perfectly suited to the study of the mechanisms underlying these pulse variations. It can be used to investigate cardiac function parameters and to localize each heart beat in the respiratory cycle. For this, it is necessary to display the airway pressure signal on the screen of the echocardiograph. By convention, we have defined heart beat 1 as occurring at the end of expiration, heart beat 2 at the start of insufflation, heart beat 3 at the plateau, and heart beat 4 at the start of expiration.
Whereas at steady-state, and throughout the respiratory cycle, the stroke volume (SV) of the left ventricle is on average identical to that of the right ventricle, mechanical ventilation dissociates these two values: the SV of the right ventricle is decreased on insufflation whereas the SV of the left ventricle is increased at the same time.
Film no. 1
TEE – View of the vessels at the base of the heart.
Pulsed Doppler in the trunk of the pulmonary artery (PA).
TEE – View of the vessels at the base of the heart.
Pulsed Doppler in the trunk of the pulmonary artery (PA).
At each inspiration, there is a decrease in right ventricular ejection.
Film no. 2
TEE - Transgastric view at 90° past the outflow tract of the left ventricle (LV). Ao: aorta.
At each inspiration, there is an increase in left ventricular ejection.
Three inspiratory phenomena are responsible for this dissociation: diminished systemic venous return, increased impedance on right ventricular ejection, and improved left ventricular filling.
TEE - Transgastric view at 90° past the outflow tract of the left ventricle (LV). Ao: aorta.
At each inspiration, there is an increase in left ventricular ejection.
Three inspiratory phenomena are responsible for this dissociation: diminished systemic venous return, increased impedance on right ventricular ejection, and improved left ventricular filling.
Media
Figure 1 : TP: airway pressure. Recording of systemic blood pressure in a patient presenting dUP
Figure 2 : TP: airway pressure. Recording of systemic blood pressure in a patient presenting dDown
Figure 3 : TEE view of the vessels at the base of the heart. Recording of pulmonary arterial flow by pulsed Doppler in the trunk of the pulmonary artery. Insertion of the airway pressure signal enables localization of the heart beats in the respiratory cycle. By definition, heart beat 1 is end-expiratory, 2 occurs at the start of insufflation, 3 is end-inspiratory, and 4 occurs at the start of expiration.
Figure 2 : TP: airway pressure. Recording of systemic blood pressure in a patient presenting dDown
Figure 3 : TEE view of the vessels at the base of the heart. Recording of pulmonary arterial flow by pulsed Doppler in the trunk of the pulmonary artery. Insertion of the airway pressure signal enables localization of the heart beats in the respiratory cycle. By definition, heart beat 1 is end-expiratory, 2 occurs at the start of insufflation, 3 is end-inspiratory, and 4 occurs at the start of expiration.