Vous êtes ici : UFR Simone Veil - santéFRFormation continueCardiorespiratory interactions01. Decreased systemic venous return
- Publié le 3 février 2023
- Version PDF
01. Decreased systemic venous return
This hypothesis has been demonstrated in spontaneously breathing patients during serious acute asthma when inspiration can result in the collapse of the inferior vena cava.
Film no. 3 : TTE – Subcostal view
Spontaneously breathing patient hospitalized for serious acute asthma.
At each inspiration, the inferior vena cava collapses where it crosses the diaphragm
Recently, we have confirmed this during mechanical ventilation, but at the superior vena cava (SVC) which is subject to intrathoracic pressure. On clamping of the inferior vena cava for hepatectomy, we first observed the occurrence of inspiratory collapse of the SVC, responsible for marked inspiratory decrease in the right ventricular stroke volume.
The longitudinal view of the superior vena cava (SVC) does not visualize respiratory variations in its size. Pulsed Doppler in the trunk of the pulmonary artery (PA) does not reveal variations in right ventricular ejection
In the same patient, clamping of the inferior vena cava by the surgeon resulted in inspiratory collapse of the superior vena cava (SVC), thereby causing a marked inspiratory drop in right ventricular ejection (*).
Patient ventilated for septic shock following pneumopathy. The TEE was done because of the persistence of arterial hypotension.
At each inspiration, there was collapse of the superior vena cava (SVC), which caused a cyclic decrease in right ventricular ejection (*).
This appearance is suggestive of hypovolemia and calls for volume expansion.
Film no. 7
In the same patient, after volume expansion, the cyclic variations in size of the superior vena cava (SVC) and of right ventricular ejection disappear.
Lastly, its presence depends not only on the volemia of the patient but also on the ventilation parameters, allowing adjustment of the volemia to a given ventilation, or even the ventilation to a given hemodynamic state.
Patient mechanically ventilated following pneumopathy.
In ZEEP, there are no significant inspiratory variations in superior vena cava (SVC) diameter or in right ventricular ejection.
In the same patient, the application of a PEEP of 5 cmH2O, needed to correct marked hypoxemia, led to inspiratory collapse of the superior vena cava (SVC), which in turn caused a drop in right ventricular ejection (*) and a lowering of blood pressure.
Media
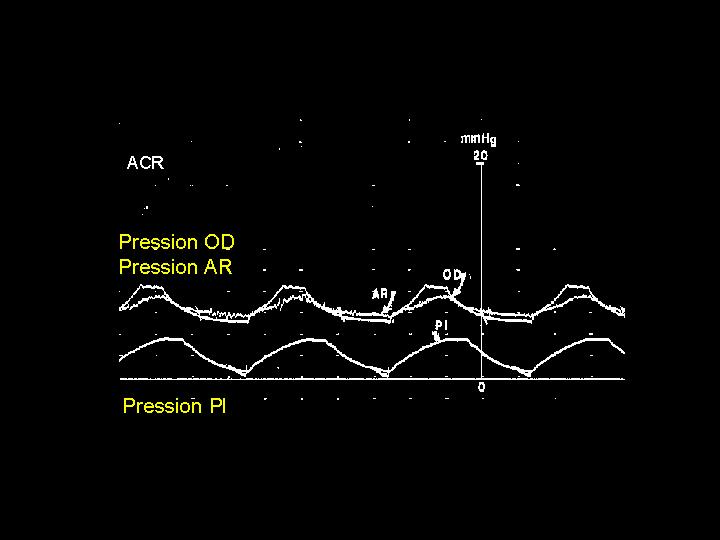
Figure 4 : Simultaneous recording of systemic arterial pressure (Pa), right atrial pressure (Pra) and pleural pressure (Ppl) in a mechanically ventilated patient, during cardiac arrest. The increase in pleural pressure, linked to the ventilation, is transmitted both to the systemic pressure and to the right atrial pressure.