Vous êtes ici : UFR Simone Veil - santéFRFormation continueSeptic shock03. Look for right ventricular failure
- Publié le 3 février 2023
- Version PDF
03. Look for right ventricular failure
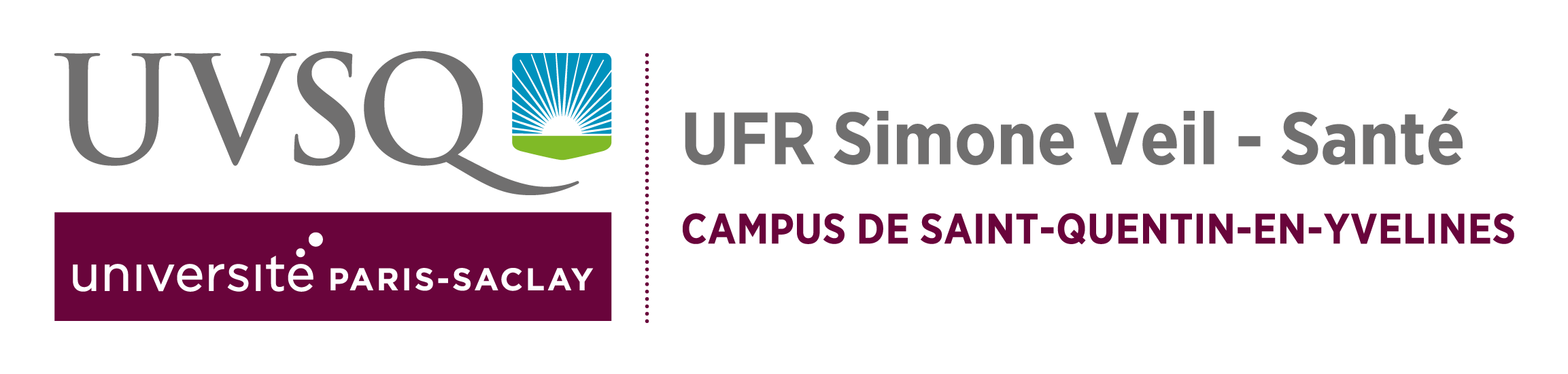
In certain situations, right ventricular (RV) systolic dysfunction may occur alone or combined and cause persistent circulatory insufficiency. This happens when there is intrinsic alteration of RV contractility, which was described in septic shock many years ago, or when there is acute cor pulmonale (ACP) due to severe acute respiratory distress syndrome (ARDS). So, in all cases in this third and last part of the examination, echocardiography should assess right ventricular systolic function. We never use RV fractional area contraction, calculated from a long-axis view of the LV (RVFAC = RV end-diastolic area – RV end-systolic area / RV end-diastolic area), because in our experience it is neither sensitive nor specific in the diagnosis of RV systolic dysfunction. On the other hand, and given the usual functional characteristics of the RV when there is low pressure circulation, any significant right ventricular failure is accompanied by dilation of the RV. This is therefore the principal parameter that we evaluate from a long-axis view of the LV which distinguishes the four cardiac chambers.
Subcostal echocardiography reveals the IVC, which often seems dilated in right ventricular failure.
RV dilation may be associated in certain circumstances, as ARDS, with paradoxical movement of the interventricular septum, indicating systolic overload of the ventricle. Right ventricular failure is then in keeping with acute cor pulmonale (ACP).
Acute cor pulmonale in a patient with septic shock due to pneumonia who developed acute respiratory distress syndrome. The long-axis view showed severe dilation of the right ventricle (which was larger than the left ventricle). The short-axis view revealed paradoxical septal movement (back-and-forth movement of the interventricular septum), indicative of systolic overload of the right ventricle.
Apart from adaptation of assisted ventilation, which will not be discussed here, the treatment of right ventricular failure, partly or wholly responsible for circulatory insufficiency, depends on the state of LV systolic function. In practice, when RV failure is combined with marked LV systolic dysfunction, infusion of an inotropic agent is required.
LV: left ventricle; LA: left atrium; RV: right ventricle; RA: right atrium
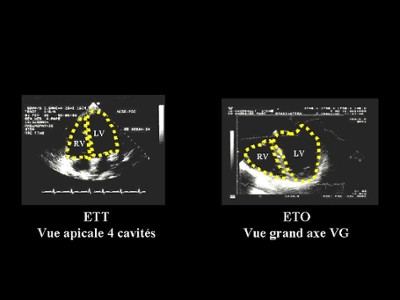
Severe sepsis of urinary origin in a spontaneously breathing young woman. Initial vascular filling in the emergency room did not correct the state of shock and worsened violent pain of the right hypochondrium which proved to be related to a cardiac liver. Transthoracic echocardiography showed :
- on the apical four-chamber view, marked dilation of the right ventricle
- on the long-axis parasternal view in M-mode, marked hypokinesis of the left ventricle,
- on the short-axis parasternal view, dilation of the right ventricle at its outflow tract and severe and global (affecting all walls) hypokinesis of the left ventricle.
LV: left ventricle; LA: left atrium; RV: right ventricle; RA: right atrium
In the female patient of Film 17, dobutamine infusion restored blood pressure to normal and resolved pain in the right hypochondrium. Echocardiography about one hour after the start of infusion showed normal right and left ventricular function.
Patient on assisted ventilation for acute respiratory distress syndrome in a setting of sepsis. TEE revealed acute cor pulmonale. Left ventricular systolic function was conserved.
Film no. 20
In the same patient as in Film 19, infusion of noradrenaline corrected circulatory insufficiency and restored right ventricular function to normal. TEE demonstrated disappearance of acute cor pulmonale.
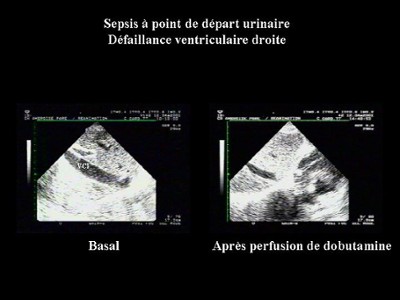
Lastly, detection of ACP is important, not only for ventilatory treatment, but also to circumvent certain mistakes in interpreting cyclic variations in pulse pressure (delta PP). Severe ACP can result in significant delta PP, and yet no associated preload reserve. In this case, the variations in delta PP are linked to a cyclic effect on RV afterload.
Patient on assisted ventilation for acute respiratory distress syndrome. This patient presented circulatory insufficiency and significant variations in pulse pressure (see figure 7) suggesting a need for blood volume expansion. In fact, these variations were related to severe acute cor pulmonale as indicated by major dilation of the right ventricle.
The same patient as in Film 21, but after blood volume expansion. Filling did not correct circulatory insufficiency and large variations in pulse pressure remained (see figure 7).
In this situation, study of SVC often avoids pointless or even dangerous refilling.
Media
Figure 5 : Method of detecting RV dilation
Figure 6 : Visualization of the IVC by the subcostal route in a female patient hospitalized for septic shock. IVC dilation, reflecting the right heart failure, is corrected by dobutamine infusion.
Figure 7 : Patient on assisted ventilation because of ARDS, presenting severe ACP
Blood volume expansion was unable to correct significant variations in pulse pressure.