Vous êtes ici : UFR Simone Veil - santéFRFormation continueAcute Cor Pulmonale03. Systolic overload
- Publié le 9 février 2023
- Version PDF
03. Systolic overload
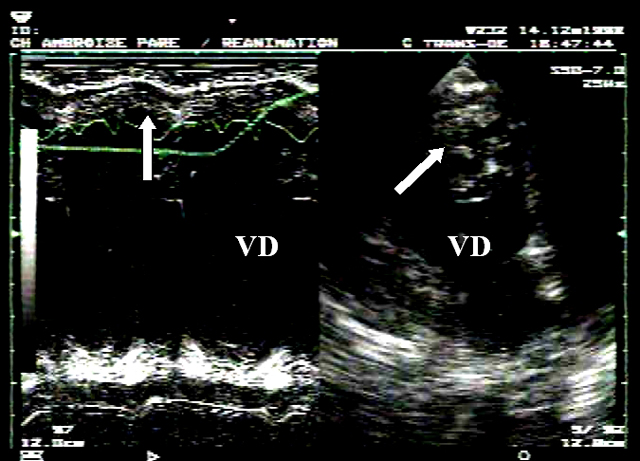
These septal anomalies are clear in a small-axis view (Figure 5), and can be analyzed in more detail in motion mode (M-mode) (Figure 1).
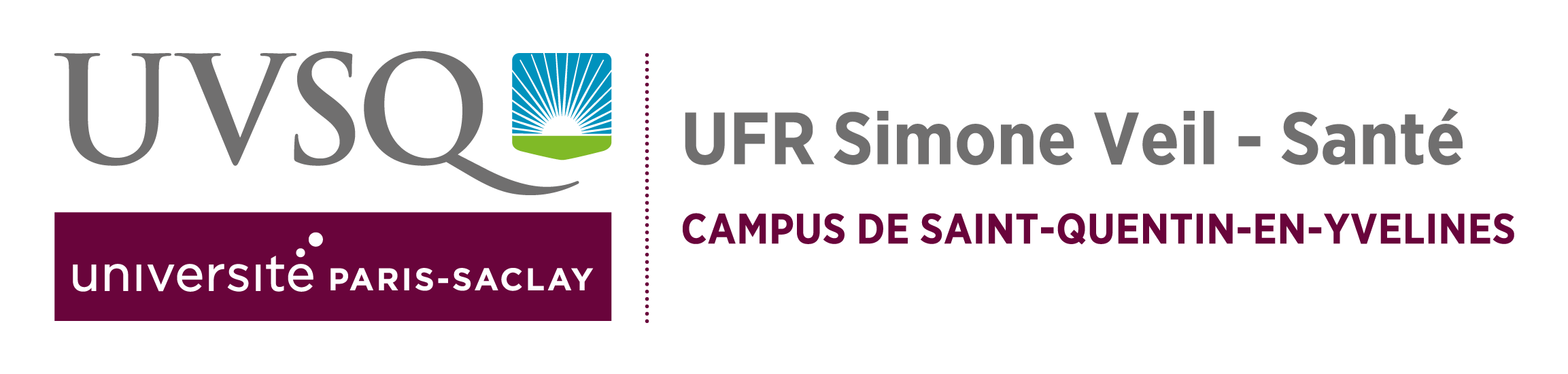
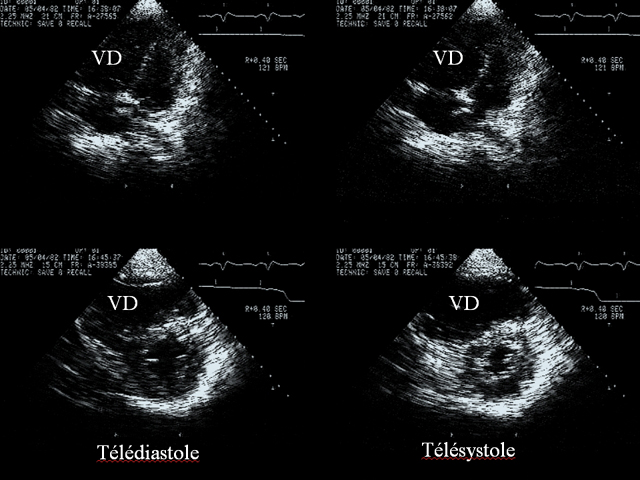
- First, the shape of the right ventricle changes. On the long axis, the apical region, which is normally triangular, becomes rounded. On the short axis, the right ventricle changes from a crescent to an oval shape. Together with dilatation, this deformation has the effect that the shape of the right ventricular chamber, which is normally very different from that of the left ventricular chamber, comes to resemble it somewhat (Figure 5).
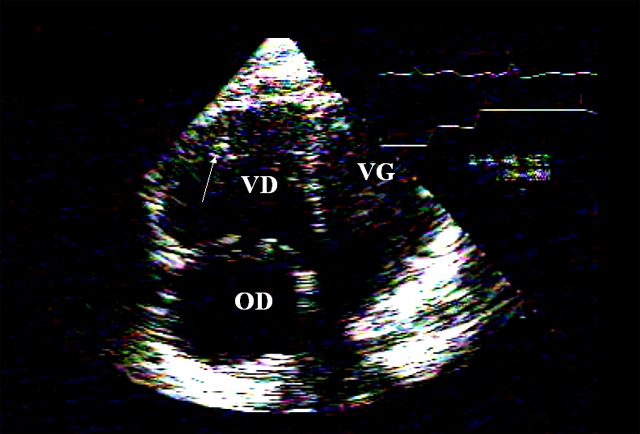
- Second, incipient hypertrophy of the free wall of the RV occurs, with accentuation of muscular trabeculae (Figures 6 et 7), and wall thickening (Figures 7 et 8). Values around 0.6 cm are common for the right ventricular free wall whose thickness normally does not exceed 0.3 cm. But parietal hypertrophy is never as marked as that seen in chronic cor pulmonale where values of about 1 cm are common.
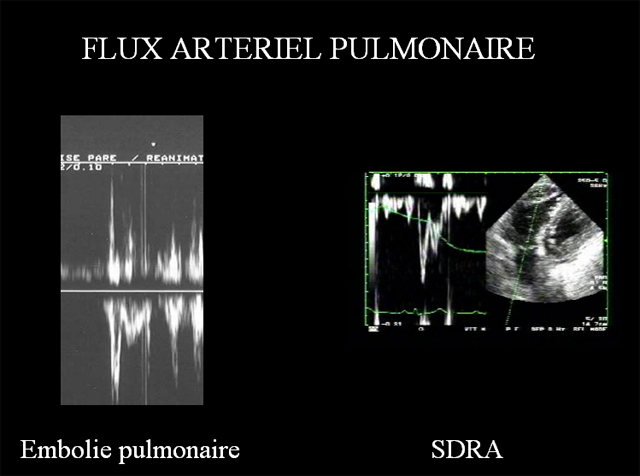
Severe systolic overload leads to a reduced ejection volume, which can be evaluated by the Doppler time-velocity integral of the pulmonary flow (table 2). A biphasic appearance indicates a large increase in resistance to pulmonary blood flow. The reduction in ejection volume is compensated for a while by tachycardia, but in the end leads to a drop in cardiac flow. The onset of ACP can therefore precipitate acute circulatory insufficiency.
The reduction in ejection volume is compensated for a while by tachycardia, but in the end leads to a drop in cardiac flow. The onset of ACP can therefore precipitate acute circulatory insufficiency.
Long-axis measurement of the right ventricular diastolic and systolic areas can be used to calculate the fractional reduction in right ventricular area. But this measurement, which is very useful when studying the quality of left ventricular systolic function, is, in our experience, of no value when studying the RV. This is because there is no fixed normal physiological value, and because pathological variations in this parameter can occur for a while in the same direction as variations in afterload.
Media
Contents
01. Reminder: ventricular independance
02. Principal echocardiographic views used to study detect ACP
03. Systolic overload
04. Diastolic overload
05. Effects of acute cor pulmonale on the left ventricle
06. Acute Cor Pulmonale complicating massive pulmonary embolism
07. Acute Cor Pulmonale complicating acute respiratory distress syndrome
08. Acute Cor Pulmonale in other clinical settings
09. References