Vous êtes ici : UFR Simone Veil - santéFRFormation continueAcute Cor Pulmonale04. Diastolic overload
- Publié le 9 février 2023
- Version PDF
04. Diastolic overload
Diastolic overload of the right ventricle dilates this chamber at the end of diastole. This dilatation is easy to observe but difficult to measure accurately. The particular shape of the right ventricle means that any volume calculation by echocardiography is impossible in practice. However, long-axis measurement of the right ventricular area is straightforward using an apical four-chamber view or the transesophageal route. It is therefore possible to establish the ratio of the end-diastolic areas of the two ventricles, which is normally less than or equal to 0.6. A ratio above 0.6 can therefore be considered as indicative of right ventricular dilatation. But this is not necessarily pathological and must be interpreted in the light of other echocardiographic signs, notably the presence or absence of a septal anomaly suggesting systolic overload. Likewise, a normal Doppler echocardiogram of mitral flow, when the RV seems slightly dilated, rules out a pathological cause. On the other hand, a E/A ratio equal to or lower than one indicates marked right ventricular dilatation and is always pathological.
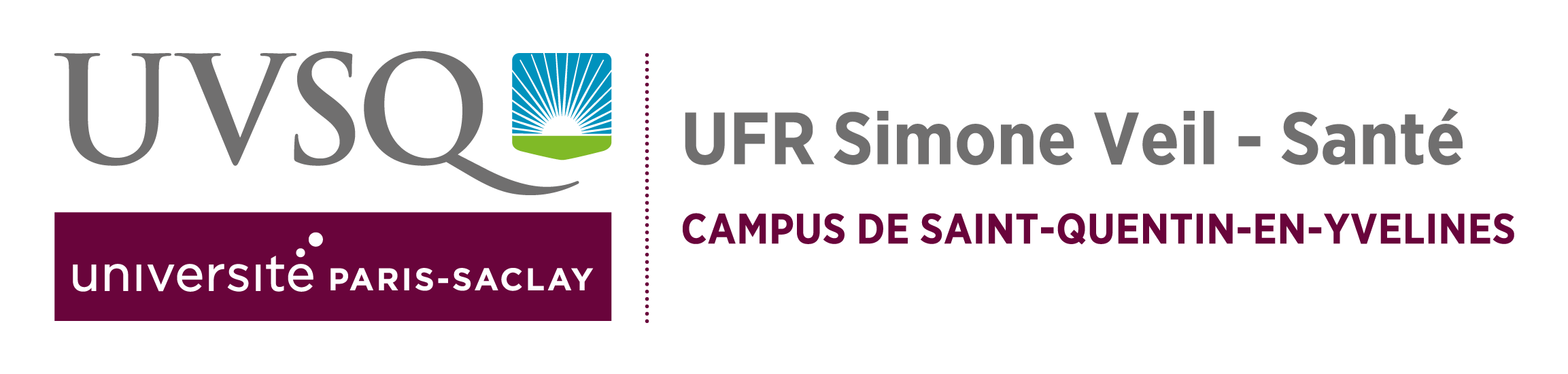
Film 7 : Transthoracic apical four-chamber view in a female patient hospitalized following massive PE. Echocardiography reveals severe ACP. In particular, the RV is considerably dilated and so crushes the LV. Note also the relative hyperkinesia of the apical portion of the free wall of the RV, described in this setting by Goldhaber. It is simply the result of the marked dilatation of the RV.
Film 8 : Patient on controlled mechanical ventilation because of ARDS caused by extensive lung involvement in varicella. TEE reveals ACP. On this long-axis view of the LV, the RV appears very dilated as its area in this plane is greater than that of the LV. The LV is subject to marked restriction and has a typical elongated “glove finger” form.
The right ventricular dilatation observed during acute cor pulmonale is associated with right atrial dilatation (Figure 2, Figure 10), and enlargement of the inferior vena cava.
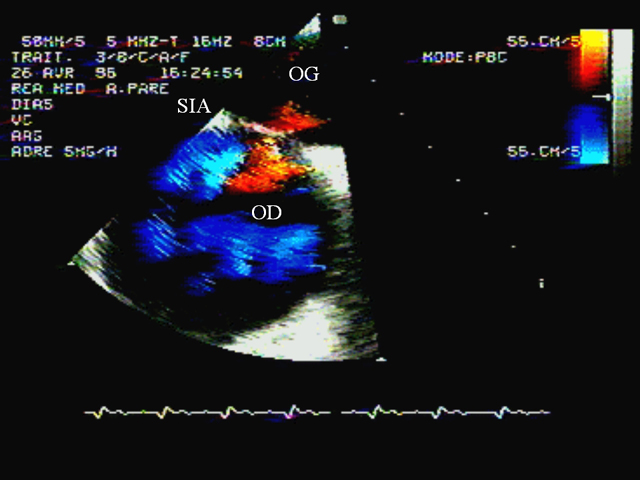
There is also tricuspid regurgitation which can be seen by contrast ultrasound (Figure 11), and which is utilized to measure pulmonary artery systolic pressure, using Doppler echocardiography (Figure 3).When right atrial pressure exceeds left atrial pressure, the foramen ovale, which had remained permeable, may reopen. This anomaly, which induces a right-left shunt, can be detected by contrast ultrasound or color Doppler (Figure 13) (5, 6). It causes paradoxical arterial embolism in thromboembolic disease (7).
Film 9 : ETO chez une patiente sous ventilation contrôlée pour un SDRA secondaire à une inhalation massive. Après plusieurs jours de ventilation, la patiente développe un CPA. L’ETO objective la présence d’un foramen ovale perméable (flux orangé), grâce au Doppler couleur, en utilisant l’image bidimensionnelle (à droite) couplé au mode temps-mouvement (à gauche).
Media
Figure 10 : Severe acute pulmonary heart in acute respiratory distress syndrome.
On this long axis view obtained from a trans-esophageal approach, note the right ventricular (RV) area greater than the left ventricular (LV) area. The right atrium (RA) is also very dilated
On this long axis view obtained from a trans-esophageal approach, note the right ventricular (RV) area greater than the left ventricular (LV) area. The right atrium (RA) is also very dilated
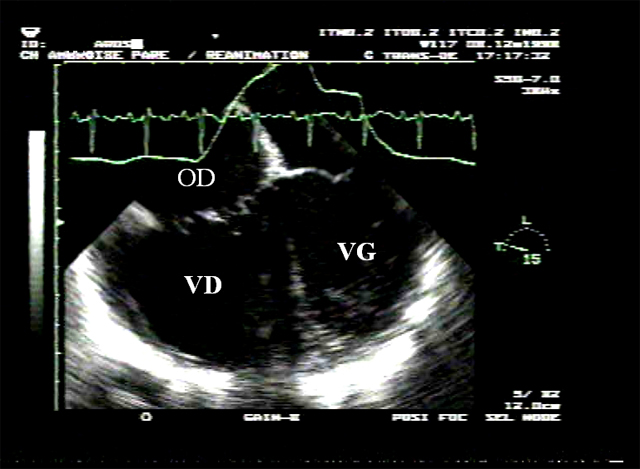
Figure 11 : Dilatation of the inferior vena cava. A: in this female patient presenting acute right ventricular insufficiency, the inferior vena cava (IVC) and a hepatic vein (HV) are dilated. B: after injection of contrast agent in a vein of the superior caval network, the agent flows back into the IVC and IHV, indicating tricuspid regurgitation.
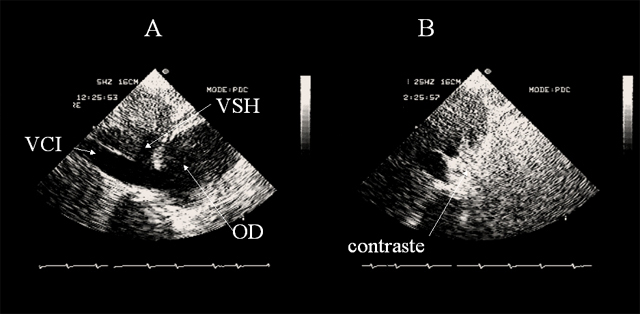
Figure 12 : Contrast echocardiographic detection of patent foramen ovale (PFO). In this patient massive pulmonary embolism is complicated by acute cor pulmonale which is indicated by dilatation of the right atrium (RA) and right ventricle (RV), with reduced left ventricular (LV) size on an apical four-chamber view (A). Injection of contrast agent in a peripheral vein (B) opacifies the right chambers, but the contrast agent quickly passes into the left chambers, indicating patency of the foramen ovale.
Figure 13 : Color Doppler detection of patent foramen ovale (PFO). In this patient presenting acute cor pulmonale complicating massive pulmonary embolism, color Doppler examination of the interatrial septum (IAS) shows turbulent flow towards the probe (red), across the IAS and into the left atrium (LA). Note also the marked dilatation of the right atrium (RA).
Contents
00. Acute pulmonary heart
01. Reminder: ventricular independance
02. Principal echocardiographic views used to study detect ACP
03. Systolic overload
04. Diastolic overload
05. Effects of acute cor pulmonale on the left ventricle
06. Acute Cor Pulmonale complicating massive pulmonary embolism
07. Acute Cor Pulmonale complicating acute respiratory distress syndrome
08. Acute Cor Pulmonale in other clinical settings
09. References
01. Reminder: ventricular independance
02. Principal echocardiographic views used to study detect ACP
03. Systolic overload
04. Diastolic overload
05. Effects of acute cor pulmonale on the left ventricle
06. Acute Cor Pulmonale complicating massive pulmonary embolism
07. Acute Cor Pulmonale complicating acute respiratory distress syndrome
08. Acute Cor Pulmonale in other clinical settings
09. References